MUMBAI: Fraud and waste proceed to pull India’s health-insurance system, with Rs 8,000–10,000 crore leaking from declare payouts annually, says a Boston Consulting Group–Medi Help report. Fraud and pointless claims inflate premiums, pressure insurer funds and drain public funds. Weak information techniques and free checks additionally push sufferers into increased out-of-pocket spends.The evaluation reveals retail well being portfolios carry increased fraud danger than group portfolios. Inside group covers, fraud is constantly elevated in BFSI and healthcare. Reimbursement claims pose the largest menace: group reimbursement claims present 9x extra fraud than group cashless, whereas particular person reimbursement claims present 20x the incidence of group cashless. Misrepresentation and doc fabrication stay the highest fraud sorts throughout IPD/OPD. Fraud danger clusters in mid-ticket claims (Rs 50,000-Rs 2.5 lakh), the place incentives are excessive and oversight average.
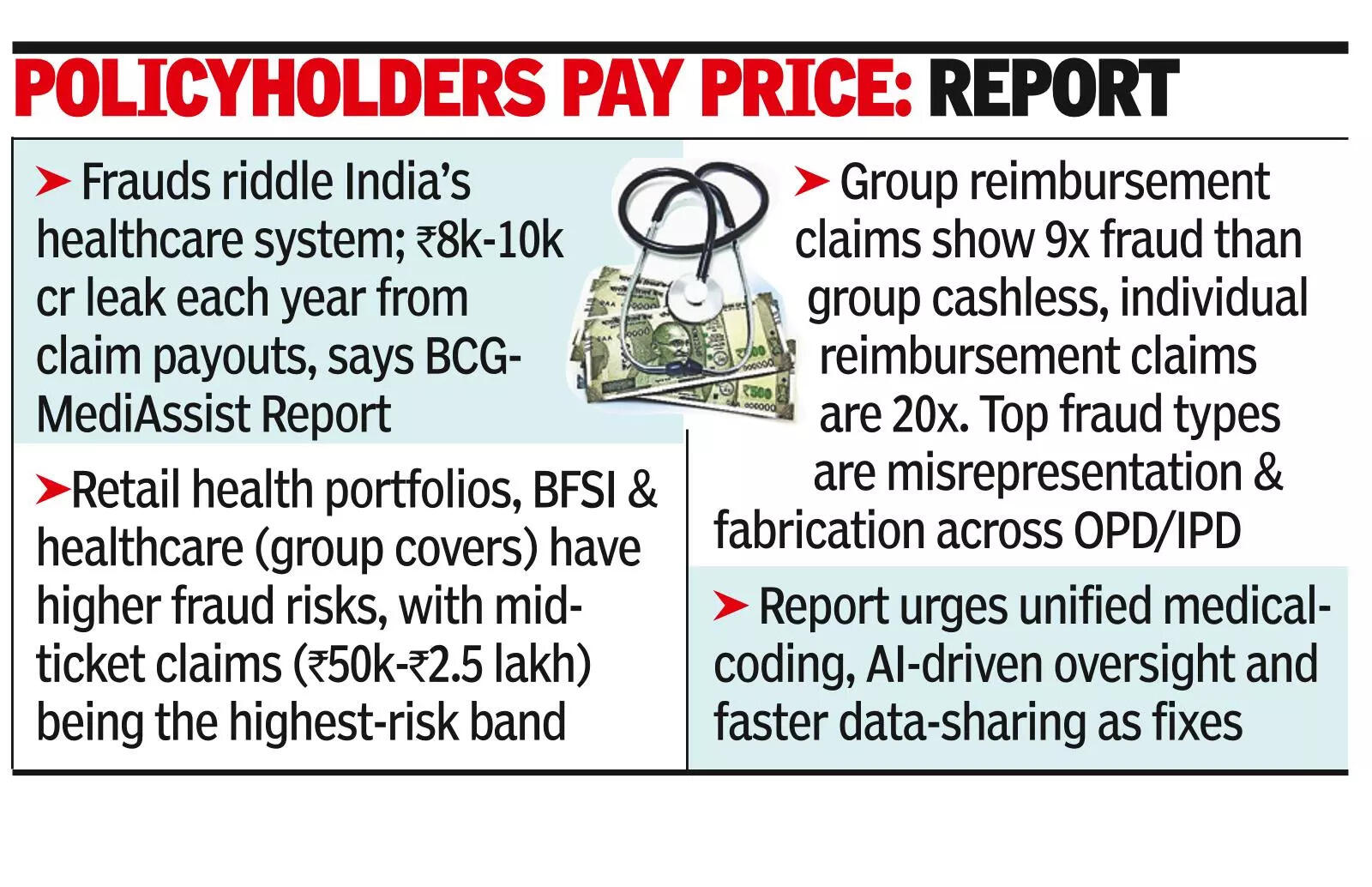
“Small-ticket fraud and abuse are sometimes rationalized as innocent… This mindset has become a systemic behavioral problem… contributing materially to the broader challenge of FWA (fraud, waste and abuse) within the medical insurance ecosystem,” the report mentioned.The report urges tighter fraud prevention/detection, unified medical-coding guidelines, AI-driven oversight and sooner data-sharing through the Ayushman Bharat Digital Mission and the Nationwide Well being Declare Change. Medi Help says tech will do the heavy lifting. “As India’s well being system stands at an inflection level, the subsequent decade can be outlined by linked information and clever automation,” mentioned Satish Gidugu, Medi Help’s CEO. Lowering fraud and rebuilding digital belief, he mentioned, will assist preserve care “accessible, inexpensive, and accountable for all residents.”For BCG’s Swayamjit Mishra, the largest beneficial properties lie within the “remaining 8%” of claims that sit between innocent and outright fraudulent.

